Automation of Claims Processing
Revolutionizing the Healthcare Industry
In an era where efficiency defines success in the healthcare industry, slow and error-prone manual processes for claims processing can hinder operational flow and affect service quality. Our solution automates and streamlines the entire claims management lifecycle, minimizing human intervention and significantly cutting down processing time and costs.
Slow Error-Prone Manual Processes
Manual handling of regulatory filings and customer orders delays crucial financial and logistical operations.
A team of 30 full-time employees (FTEs) processes over 25,000 monthly claims through labor-intensive re-scanning, leading to significant delays and potential errors in data handling.
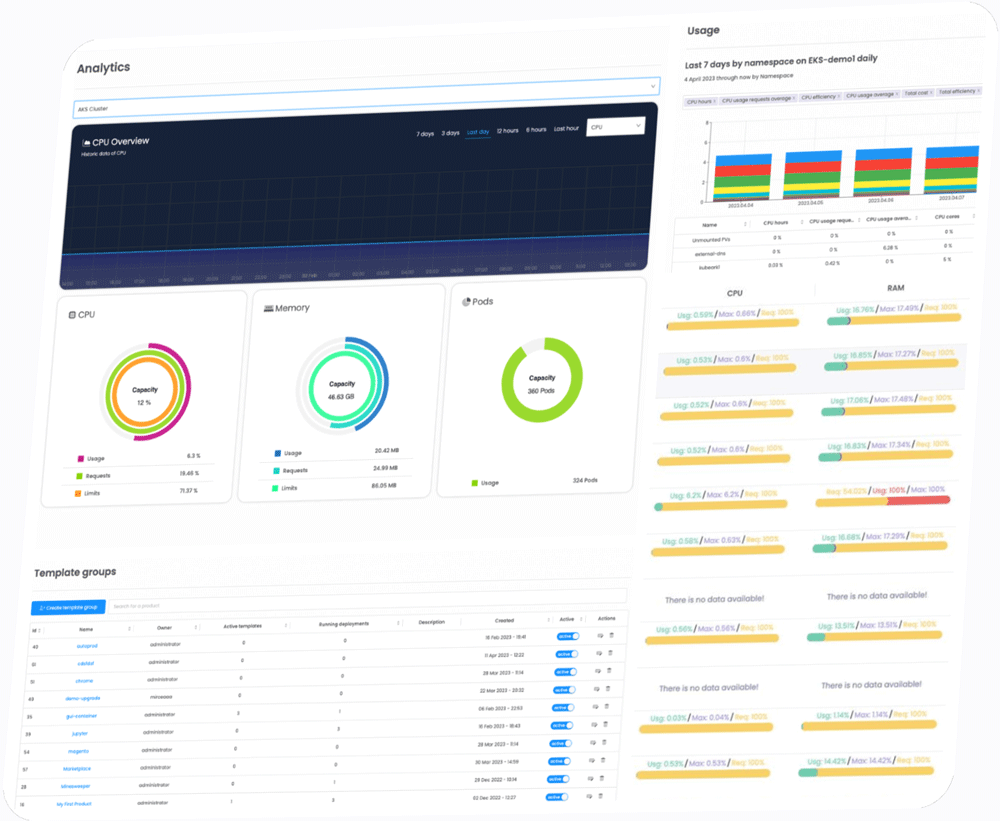
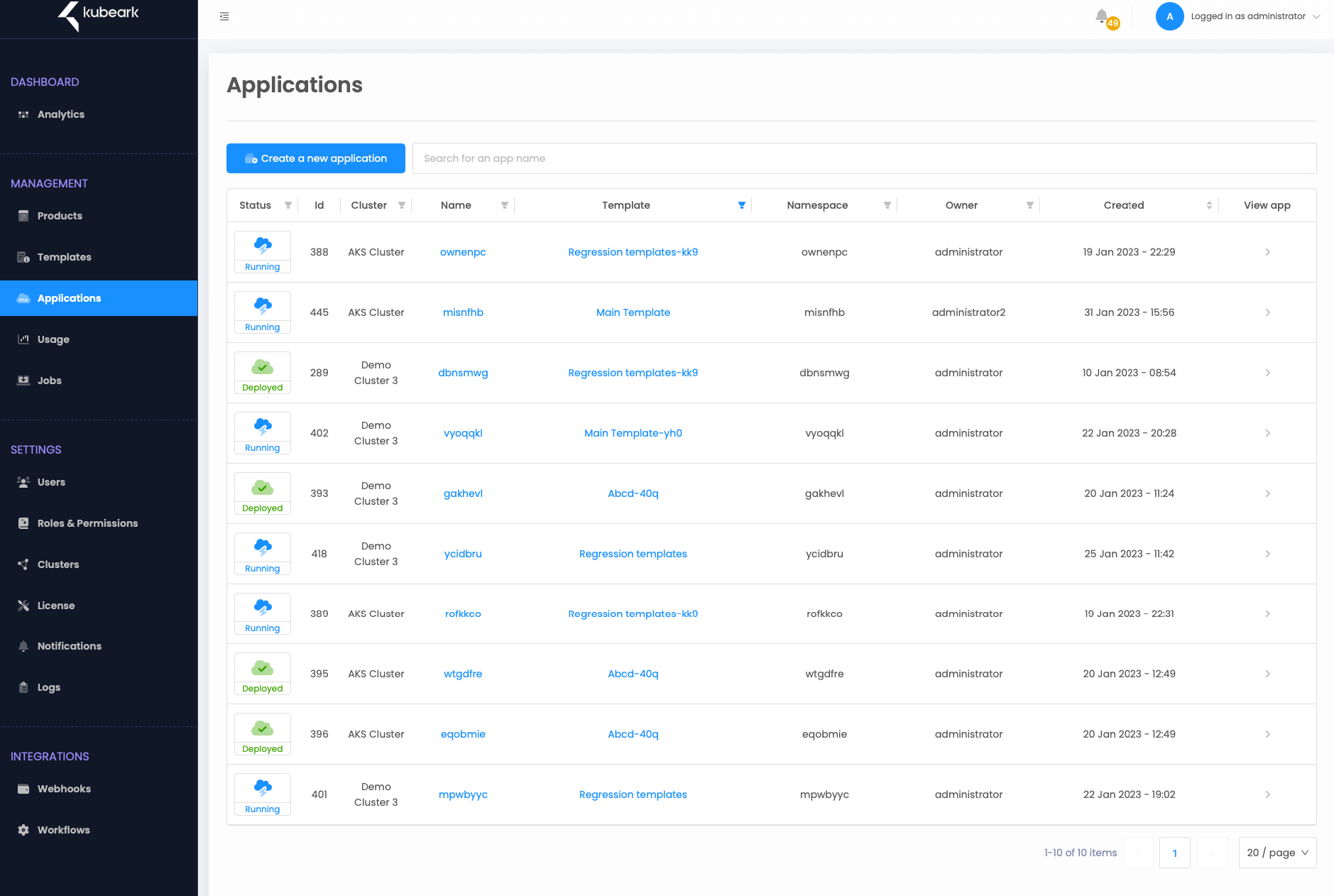
The Kubeark Solution
Transforming Claims Processing with State-of-the-Art Automation
Kubeark's platform integrates seamlessly with any Electronic Health Record (EHR) systems to eliminate the need for PDFs in the workflow, allowing for direct data exchanges between insurers and medical partners.
This integration results in a substantial decrease in both processing times and manual tasks, dramatically improving overall operational efficiency.
Reduce Human Error and Increase Processing Speed
With automated systems, the accuracy of claims processing improves while the time required for processing each claim is reduced.
Streamline Claims Processing
Accelerate the entire claims lifecycle from submission to settlement.
Improve Regulatory Compliance
Ensure claims are processed in compliance with current healthcare regulations and standards.
Enhanced Coordination and Data Sharing
Automated systems facilitate better data integration and coordination between medical partners, leading to faster and more accurate claims reconciliation and payment.
Up to
€234K
Saved Annually in FTE Costs
Automation reduces the need for extensive manual labor, leading to significant cost savings.